How I Cured My Perioral Dermatitis—The Skin Condition You’ve Never Heard Of and How I Learned to Manage Mine
⏱ 17 min read | Audio version below
February 22, 2024 Update:
It’s been a year and a half since I first published this blog post. It continues to be one of my most widely shared pieces, blowing up my DMs each time it has a viral moment. In response to readers’ questions, I thought I’d give you an update on how my skin is today and what products I am currently using!
As you can see, my skin is still clear and smooth nearly five years after my diagnosis of perioral dermatitis (PD). Much of my regime remains the same. Here are the exact products I now use on my face each day:
Herbal Face Food’s The Serum III. Now that my flare-ups are consistently under control, I upgraded from the antioxidant potency of The Serum II to the more potent Serum III, pressing a dropper-ful into my skin each morning.
Herbal Face Food’s The Cream or Supergoop’s Glow Screen. The Cream has an SPF of 50 as well as powerful anti-aging botanicals. It’s what I wear most often but on days that I want a shimmery makeup look—without wearing a stitch of foundation—I’ll smooth on Glow Screen in the tinted shade called Sunrise.
Typology’s 7-Ingredient Cleansing Oil. When I wash my face at night, this is what I use to remove makeup and sunscreen. I love how it doesn’t dry out my skin.
Rice water. I make this toner myself (see recipe below), soaking it into a cotton pad and dabbing my face after cleansing to remove any residual product.
15% Azelaic acid gel and Altreno 0.05% lotion. I alternate between these topical prescriptions every other night. One night, I’ll use azelaic acid to help keep PD flare-ups at bay. The next night, I’ll use Altreno, a tretinoin lotion that helps prevent wrinkles. I’m 38 now, after all.
That’s it! If you’d like to try any Herbal Face Food products at 20% off, use coupon code ALICEG20 at checkout. They remain the only company I have an ongoing affiliate partnership with.
Hope you found this helpful and cheers to your skin recovery journey!
This essay is available in audio format.
See those tiny bumps in my before photo? Not the big ones—the other ones that might be described as “rough texture”? Each of those little bumps would balloon into full-sized pustules over the course of a month, like all the bumps before them and all the bumps after. My scars would fade just in time for new bumps to come in. Every month was the same for six miserable years.
I thought it was acne. It wasn’t.
That clear, smooth skin you see in the photo to the right? I want to cry looking at it. This before-and-after set looks like one of the hundreds I used to pour over during late-night internet searches. You know, the too-good-to-be-true sets with the slightly blurrier after photo that’s obviously been filtered, like we, the desperate, can’t tell. But I took the photo on the right. I made this set, and although you’ll have to take my word for it, I know it’s not altered. If anything, the quality of my after photo is even sharper than the before one. And it’s mine.
My skin struggle...
Anyone with acne knows the dread of scanning your face for new zits each morning. Just when your scars seem faded from your last breakout, you get a fresh crop of pimples, painful to the touch and so embarrassing you don’t want to leave the house.
I’m an actress and model. I’ve had “problem skin” since I was 12. Video shoots broadcast my face to the world in pore-revealing, high-definition close-up. Makeup only covers so much. I’ve been on sets and heard the director say, “What’s that on her face? Is it a crumb? Can someone tell her to wipe her mouth?” I’ve overheard them tell grips to arrange the lighting so dome-shaped shadows aren’t cast over my chin. I’ve apologized to actors before a makeout scene, asking them to please kiss me lightly so the layers of concealer and powder around my lipline won’t rub off with their stubble—or worse, pop the whiteheads waiting to burst.
One of my meltdown moments came when my agent sent me an audition for a toothpaste commercial. She said to bring my toothbrush because casting would be getting closeups of me brushing my teeth and showing off my beaming smile. This is what my face looked like that day:
“And that’s WITH makeup,” I emailed my agent. We both agreed I would pass. No one wants to buy toothpaste from a girl with bumps around her mouth.
Attaining good skin was my job, my livelihood, my self-esteem. I spent over two decades and tens of thousands of dollars trying everything I could to make my skin healthy—and when I say everything, I mean over-the-counter topicals, prescription oral medications, expensive laser treatments, natural enzyme peels, bloody PRP facials, acupuncture, a vegan diet, a gluten-free diet, an anti-inflammatory diet, handheld light therapy tools, and nearly every medical spa procedure under the sun. I even went through two rounds of Accutane. The last-resort medication definitely helped, but when my acne came back at age 28, it came back with a vengeance. This time, I broke out only around my mouth. Cute.
Except it wasn’t acne.
I was 33 and in the midst of a holistic facial when my aesthetician at EgoDerm, a clear-skinned beauty named Sanaa, paused her extractions on my ravaged face.
“I don’t think this is acne,” she said.
My brow furrowed beneath a washcloth. “What do you mean?” I asked.
“Usually there’s a seed,” she said, pressing harder around my popped zit while my eyes watered. “But these just have clear fluid.” Sanaa paused. “I think you have perioral dermatitis.”
Perio-what?
When my facialist told me I had blisters, not pimples, I didn’t think she knew what she was talking about. (Sorry, Sanaa!) In all of the skincare treatments I’d gotten over the years, I had never even heard of perioral dermatitis. No medical spa’s brochure ever mentioned it, no dermatologist ever suggested it, and none of my friends ever brought it up during venting sessions about our skin woes. I wish I could tell you that I asked Sanaa to write it down for me, but I didn’t. My skin kept getting worse.
Months later and beyond frustrated with the painful red bumps covering the lower corners of my mouth and my upper lip area, I came across the term again. “Perioral dermatitis,” WebMD said, “is a facial rash that causes bumps to develop around the mouth… The condition is most commonly seen in young women (90% of cases).”
I found a dermatology office with perioral dermatitis listed on their site and booked an appointment ASAP. Then, like a good self-diagnosee, I dove into Google to learn about the skin condition I was convinced I had. My formal diagnosis days later confirmed I was right. (And so was Sanaa.)
I had symptoms of perioral dermatitis for six years. It took only four months for those symptoms to vanish. Today, three years since my diagnosis, I want to share with you what I’ve learned about perioral dermatitis, why it can be so hard to manage, and what finally worked for me. My hope is that you won’t waste any more of your precious time—and your self-esteem—worsening a delicate skin condition so often mistaken for something else.

What is perioral dermatitis?
Perioral dermatitis (PD) is a condition that literally means around-the-mouth skin inflammation. When it spreads to areas beyond the mouth, such as the eyes, nostrils, and occasionally the genitals, it becomes periorificial dermatitis—skin inflammation around orifices.
Perioral dermatitis is best described as acne meets rosacea. Treating one usually exacerbates the other. Also described as eczema meets acne, PD is a bumpy or scaly rash usually presenting as clusters of red or flesh-colored bumps around your mouth and nose, or, as in my case, whitehead-like pustules. My rash of bumps was limited to my mouth area and did not burn or itch like some PD sufferers. Still, it was painful to the touch and sore to the smile.

How common is perioral dermatitis?
Hard data on the frequency of PD is difficult to come by, ranging from “0.5-1% of people in industrialized countries” to “1 in 100 women at some point in their lives.” What everyone seems to agree on is this: 90% of people with PD are women, usually between the ages of 15-45. Onset of PD typically peaks in our 20s and 30s. The development of a pimply rash around my mouth at age 28 was right on time.
What causes perioral dermatitis?
Steroid creams. Spicy foods. Sampling too many face masks, changing your makeup routine, using fluoridated toothpaste, sulfate shampoo, essential oils, French fries, hot coffee, sunshine, wind, concealer, laundry detergent. The better question: What doesn’t cause perioral dermatitis?
Before your overwhelm turns to tears of defeat, let me just say that the cause of PD is different for everyone. Fries or a day at the beach might not trigger your rash to flare up, but maybe drinking a piping hot latte or using makeup remover wipes will. Narrowing down the root of the problem requires time-consuming trial and error. Don’t fret—there is good news and I’ll share it in a moment.
How is perioral dermatitis treated?
PD is notoriously difficult to treat. The first obstacle is people’s lack of awareness about it—as I mentioned, not one of the dozens of dermatologists I saw even suggested I had PD. Many doctors treat their patients for what looks like acne. This often worsens symptoms with harsh, drying ingredients that aggravate the hypersensitive skin of a person with undiagnosed PD. Once diagnosed, however, treating PD becomes a lot more manageable.
The primary goal of treating PD is to calm the skin by reducing inflammation and eliminating irritants. In this way, PD resembles rosacea. Many causes of rosacea flare-ups also produce PD flare-ups. Alcohol, sun and wind exposure, caffeine, and common ingredients in makeup and skincare products, like mineral oil and added fragrance, are unsuited to the sensitive skin of PD and rosacea sufferers. Because every individual responds differently to treatment, I can’t tell you that what worked for me will work for you. But at least you can be better informed if you do seek a PD diagnosis. If you already have a diagnosis, I hope you can glean some helpful tips.
How I cured my perioral dermatitis…
I’ll admit that it may be a misnomer to use the word cure for how I eradicated my PD symptoms. Technically, I still have PD. It’s one of those conditions, like rosacea, that may never go away. But it can be managed effectively with medication and lifestyle choices. Here’s what worked for me in three steps.
Step 1: Get a diagnosis and take your prescriptions
No natural remedies here, folks. Living in an unnatural world sometimes requires unnatural solutions.
I saw Jessica Kramer, PA-C of the Dermatology and Laser Centre in Studio City, California. Yes, I’m giving away the name of my dermatologist because she’s that good and I can’t keep such a life-bettering secret to myself. Jessica confirmed my suspicion of perioral dermatitis on our first visit. Time and treatment would tell for sure, she said, but my symptoms were consistent with other cases she’d treated.
Jessica prescribed me two medications: an oral antibiotic called Seysara and a topical 15% azelaic acid gel. Seysara belongs to the tetracycline family. It’s often prescribed to treat stubborn acne by calming inflammation from the inside out. Azelaic acid is often prescribed to treat rosacea, especially rosacea that presents as bumpy skin. It works by calming inflammation from the outside in and reduces scarring by aiding cellular turnover.
I took 100mg of Seysara per day for six weeks. I smoothed azelaic acid gel on my face morning and night. Two months later, I didn’t see any progress. Jessica acknowledged during my follow-up visit that perioral dermatitis can be stubborn to treat, especially in the beginning and when flare-ups are at their peak. She prescribed one more round of Seysara, told me to keep using azelaic acid, and reemphasized the advice I really didn’t want to hear: eliminate, eliminate, eliminate.
Step 2: Eliminate irritants
This is perhaps the most challenging and crucial step of all.
I already told you the aggravators of PD range from spicy foods to toothpaste to mineral oil. The list of no-no’s Jessica gave me was overwhelming. But remember I said there was good news? Eliminating irritants actually works. While it’s hard to break habits we hold dear, I think radical elimination was the simple yet drastic step that allowed my PD to finally begin healing. When my skin wasn’t actively fighting irritants, the medicines started doing their job.
I didn’t want to swap my hot coffee for iced or ask for mild curry when I wanted medium. I didn’t want to stop dabbing Mario Badescu’s concealing pimple cream that, despite not working for me, at least covered my red bumps with white paste so my boyfriend wouldn’t see them. I certainly didn’t want to stop wearing makeup. But after two months of taking my prescriptions and seeing no progress, I surrendered to the recommendation I was most reluctant to try. I swapped my Mrs. Meyers detergent for Seventh Generation Free & Clear. I traded Crest 3D White for fluoride-free JĀSÖN Sea Fresh. I bought a sun visor—a semi-cute one from Urban Outfitters—and I committed to being alcohol-free at least ’til Christmas. Most drastically of all, I eliminated ALL skincare products.
I went cold turkey. No more face wash, no more serums, no more moisturizer, and—gasp!—no more concealer. Or sunscreen. The only thing I put on my face was the 15% azelaic acid gel prescribed to me by Jessica and rice water. (To be clear—Jessica advised sunscreen. I stopped sunscreen of my own volition and against doctor’s orders. Fuck balance, I’m an extremist.)
Rice water is a natural cleanser used in Asian beauty rituals since ancient times. It’s rich in amino acids and antioxidants that help calm inflammation and slow down aging. The best part is that it’s cheap and super easy to make—just mix one part rice with one part water, let it soak overnight, and then strain the liquid into a bottle. I kept my bottle of rice water in the fridge and each evening, I’d soak a cotton pad with its milky coolness and gently dab my face—dab, not rub, because the last thing any dermatitis needs is aggravation. Rice water became the only cleanser I used for two years. If I wore eye makeup, which I only did a few times, I used makeup remover on my eyes only and rice water for everything else.
And then it happened. One day, a few weeks after my radical elimination, I literally woke up with clear skin. Smooth skin. The kind of skin I dreamed of since I was twelve. I stared at my mirror in disbelief. After six years of greeting the day with tiny new bumps that flared into painful blisters, I couldn’t find a single one.
I was diagnosed with perioral dermatitis on April 11th, 2019. By August 24th, my skin was clear. It took four and a half months of medicated treatment and product elimination for my skin to transform from inflamed to calm, pustule-ridden to smooth, and sore to soft. [Click to Tweet]
See my makeup-free, unfiltered pics for yourself (and pardon the inconsistent lighting):

Step 3: Maintain and adjust when necessary
Eight months later, my skin was still clear. In fact, it had never looked better.
All I did was maintain my minimalist regimen. The beginning of the pandemic allowed me to continue not wearing makeup, and because I started taking more walks outdoors, I cautiously added sunscreen to my otherwise rigid skincare routine. I took Jessica’s recommendation and used Elta MD’s Tinted SPF 46. Elta MD’s is a barrier sunscreen, also called a physical sunscreen, as opposed to a chemical sunscreen. It’s ideal for sensitive skin that’s rosacea-, acne-, and dermatitis-prone.
I slowly added spicy foods back into my diet. I sipped hot coffee a few mornings in a row. Seeing no adverse effects, I started drinking red wine, a notorious rosacea and PD aggravator. I was quarantining with my parents after a breakup and red wine was going to be had, flare-up or no. A flare-up never came.
For blissful, blemish-free months, my healthy skin maintained. My only complaint was dryness. I missed my fragrant skin oils, my indulgent face masks, and my wrinkle-fighting serums. When I ventured to use a cream labeled safe for sensitive skin, I found the line by crossing it. Two days of use made telltale bumps appear near the corners of my mouth. It was a baby flare-up, nothing like I’d had before. Even one or two pustules is now one too many for me. Not when I know flawless skin can be mine with a little discipline. (I have since found a moisturizer that I LOVE and I’ll share it with you momentarily!)
A year passed. I fell in love and started having fun again as the world slowly reopened. I learned too much sun and tequila, combined with little sleep, triggered mini PD flare-ups. When modeling jobs picked back up, makeup and travel didn’t do my skin favors, either. I took to bringing my own concealer, a Make Up Forever HD Stick Foundation that I blended with my Elta MD sunscreen, and I avoided alcohol and spicy foods whenever work or castings were on the horizon.
A routine follow-up with Jessica told me I could take doxycycline as-needed. Whenever I first noticed signs of a flare-up, usually after a week of poor sleep or overindulging, I could take 50mg of the antibiotic once per day for about a month. I’ve only ever needed two courses.
Then, this past winter, it seemed like my routine was no longer working. Tiny bumps were turning into big bumps once more. I scheduled an appointment with Jessica in a panic. I didn’t know what was causing the flare-up this time—was it my new shampoo? The spicy laab from Same Same Thai? Stress?
Jessica refilled my doxycycline prescription, but, not wanting to keep relying on an oral antibiotic, I asked her about a medication called Soolantra. Soolantra is a rosacea cream that works by—brace yourself—killing the Demodex mites that live in our skin. We all have them. People with rosacea often have 15-18 times more. Because perioral dermatitis is so closely related to rosacea, many PD patients have cleared up their skin using Soolantra. Its active ingredient is ivermectin and if that makes you think of Joe Rogan, it’s because the podcaster made this antiparasitic drug famous by taking it when he got Covid.
Soolantra worked. Ten days in, I started experiencing the infamous Demodex die-off, when the microscopic bugs living in my skin (and yours) caused a flare-up of bumps as they began to die, expunged from my pores. Only thanks to the good people of Reddit did I refrain from rushing to Jessica’s office in hyperventilated tears. The die-off phase would pass in a week or two, the kind folks of the interwebs promised me. So hang in there, I did.
It got better. My skin was clear and smooth one week later.
My skincare regimen today…
Ready, guys? My daily skincare routine now boils down to this:

I start my morning by gently pressing Herbal Face Food Serum II into my skin—this is the moisturizer I love that I said I’d come back to, and I’ll tell you more about it in a moment! Once absorbed, I smooth on Elta MD Tinted Sunscreen, followed by any eye makeup I might wear that day—I never wear foundation and use my Make Up Forever HD stick as concealer only when I have shoots. In the evening, I wash my face with Typology 7-Ingredient Cleansing Oil, which I’m pleased to say doesn’t irritate my skin. I still cleanse with rice water on days I don’t wear sunscreen, but it’s summertime, so I’m wearing sunblock almost daily. Lastly, I apply a dime’s worth of prescription Soolantra cream to my face each night before bed.
That’s it. These four products are my sole skincare regimen. My skin has never been better.
I’d like to spend an extra moment telling you about Herbal Face Food. Full disclosure—they gave me an affiliate link because I like their serum so much. Completely plant-sourced with over 50 botanical concentrates in their ingredients, Herbal Face Food is a sensitive skin owner’s dream. It has the luxurious look of a fancy oil in a matte glass bottle of cobalt blue and absorbs like a medical-grade serum as potent as any prescription I’ve taken. Not only did Herbal Face Food not trigger a single PD flare-up—it made my dehydrated skin positively glow. The results speak for themselves, even in the harsh brightness of direct sunlight.
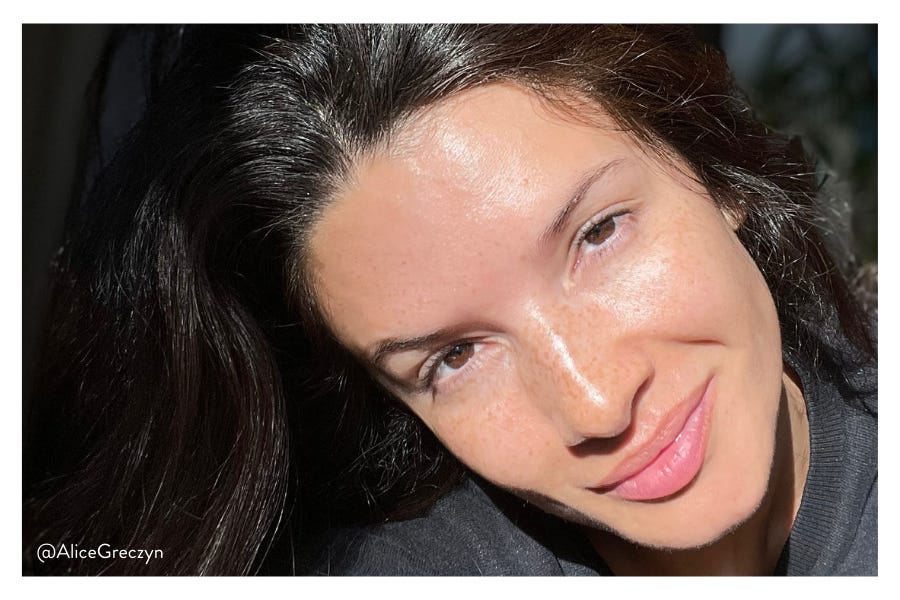
Who needs foundation with skin this perfect?! Yes, I brag—I’m damn proud of how hard I persevered to get here, and so grateful for the medical advice and products that helped me along the way. You’ll need to see your derm for prescription meds, but if you’d like to try Herbal Face Food’s serum, I have good news for you. It’s only $65 and you get 20% off any product when you use code ALICEG20 at checkout. I truly wish I’d found this product years ago. It would have saved me so much irritation from all the expensive designer creams and oils I tried. I know I know, I sound super salesy right now. But please trust me when I say—I would never steer you wrong. Especially when it comes to skincare. I’ve never had a single affiliate link, ever, and I am sincerely proud that Herbal Face Food is my first.
My journey with perioral dermatitis isn’t over, but I’ve learned what it takes to manage it. After eight years of trial and error, and three years of experimentation since my diagnosis, my hope is that you can take inspiration from my story to find your own path to healing. Call up your dermatologist, or better yet, see mine if you live near L.A. Take your prescriptions and eliminate irritants even though it’s overwhelming. When you feel like trying out products again, protect yourself with Elta MD sunscreen and nourish your skin with Herbal Face Food. Let me know how it goes because I’m convinced good skin is possible for you, too!
This newsletter is free because I think helpful information should be free as much as possible. Please subscribe, and if you’d like to donate to my costs (news subscriptions, image licensing, paywalled academic papers, etc.), I’d surely appreciate it. Thank you!











Kojic acid tumeric soap worked for me.
Thank you! So I want to make sure, is the ivermectin the one that you think truly cured the perioral dermatitis? I'm currently on metronidazole cream and it's helping the acne but not the redness around ym nose. I hated the antibiotics. Would you recommend the ivermectin for get rid of it once and for all?